The NTH Outreach Team is excited to announce the upcoming launch of our podcast, NeuroTech Roadshow. Beginning in November 2025, we will be publishing one podcast episode a month featuring industry experts, thought leaders, patients/patient advocates, and more to raise awareness of neurological disorders and facilitate the sharing of knowledge to accelerate neurotechnology advancement. The podcast will dive into topics including the neurological disorders that affect 1-in-3 people worldwide, cutting edge neuromedical interventions (both invasive and non-invasive), lived patient experience with neurological disorders, the ethics of neurotechnology, and more.
The Outreach Team is currently planning the first six episodes of the podcast, to be published from November 2025 through April 2026.
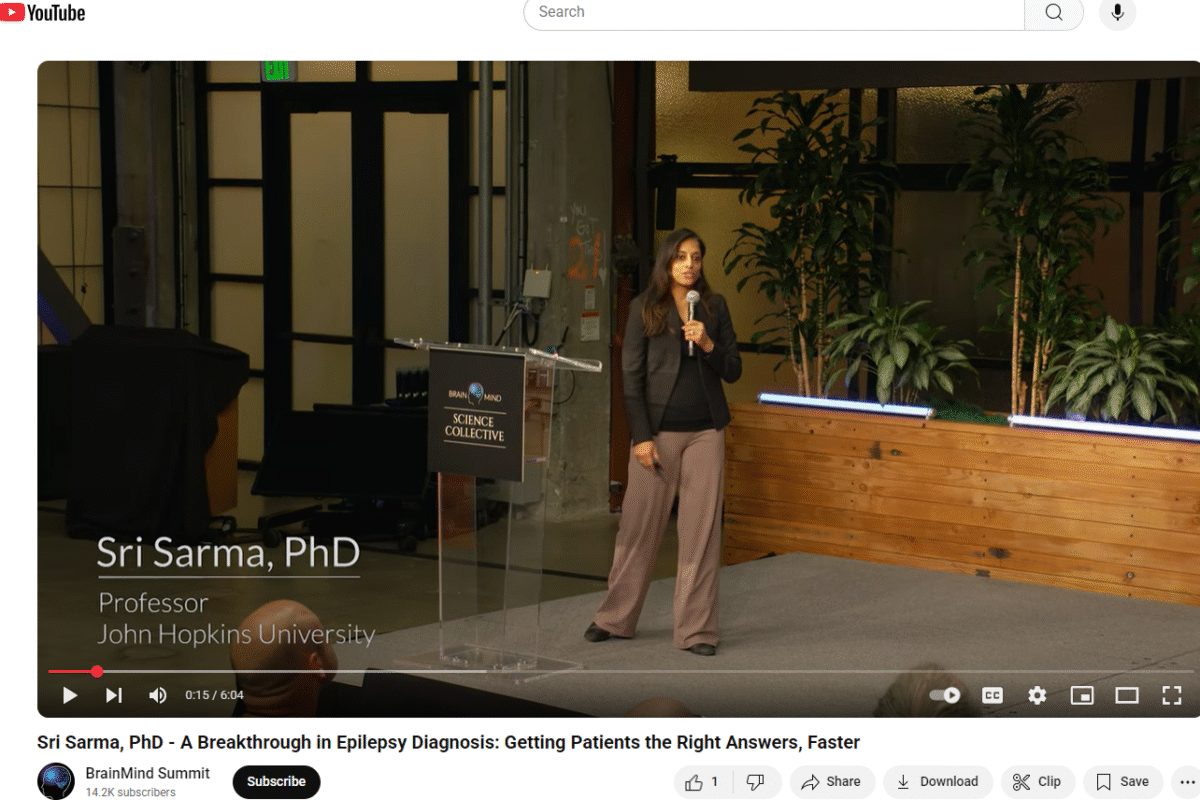
Episode one will feature Dr. Prasad Shivalkar, UCSF, and one of his patients from a clinical trial that was featured in the NYT. Episode two will feature Dr. Sri Sarma and her research into misdiagnosed non-epileptic seizures.